SUMMARY
We are now seeing less viral spread in the UK, and so falling admissions and deaths though globally the picture is mixed.
- Lockdown, immunity and vaccination means that right now in the UK the virus cant find non-immune hosts
- It is possible this is the end of the pandemic phase but new variants, global inequity and mass movement may cause problems.
- Vaccination is better than we thought at protecting against illness and transmission, and vaccine hesitancy is falling.
- The £271bn cost of the pandemic (so far) in the UK is equivalent to £9,700 per household. Novel thinking will be needed to address this, learn lessons from the pandemic and address future challenges.
Introduction
Well, here we are on the downslope of the third wave in the UK and elsewhere. With vaccination rolling out and the first hints of spring there is much in the way of optimism in the air.

End of tunnel time??
Of course, our Government is hoping this is third time lucky with previous lockdowns being lifted too early. This time they are actually following the advice from scientists in terms of not rushing ahead too quickly. I guess after the experiences last year, the chaos around Christmas, and that the big third wave which played out just as predicted by the experts gave credence to the scientists arguments that this has to be done slowly.
So this time Bo-Jo and his chums are more minded to deflect the calls for a a faster return to what we used to call normal and what we will now call the post COVID world. We will plod on with the pandemic measures for some time more, but at least, one year after the first case, there is hope.
Where are we
I remember back in October when cases started to increase reflecting that it was going to be a long winter and it has been, but perhaps the end now seems in sight. I can’t help but remember that it is just about a year since the first case in the UK, so the conditions then were right for a surge in cases, so complacency is not based on sound foundations. The virus can surprise us again.

UK COVID Hospital admissions – Is the End now in sight?
The encouraging pattern seems to be repeated across the western world – there are exceptions but generally the trends seem to be in the right direction.

However, in our unequal world, this pattern is bound not to be universal and some countries continue to struggle. Czechia is in the midst of a crisis. Brazil still reports a worrying number of deaths and the variant detected in Manaus may have re-infected those infected in the first wave, easily overwhelming their health systems and demonstrating what happens when health systems are overrun.
There seems a paradox in Africa who have been hit less hard than was initially expected, but 100,000 deaths and overrun hospitals in hot spots is still a sad matter. It might be that they are a young continent with a median age of 18 versus 40 in the UK, but that is not the whole story. The variant first detected in South Africa is spreading north so that will complicate matters too.
This is important as we have a global pandemic and in a way the important number is the total global population of viruses, which though falling, is nowhere near reaching the levels where containment becomes practical.
There are enough viruses replicating away in their human hosts for mutations to occur and enough human interconnectivity for them to spread. In many countries, public health is far from able to deal with outbreaks which always have to be expected, lockdowns are not possible and medical care is limited, ripe conditions for mutation and spread.
Added to this is vaccine Imperialism which has led to 10% of the worlds nations have consumed 90% of the vaccines so far and many countries are a long way away from vaccinating their at risk and health care groups. WHO appeals for the world to vaccinate at risk groups and health workers have not been heeded but COVAX is slowly taking up the mantle with the first 600,000 Astra Zeneca doses arriving in Ghana this week.
Here are just a few nations not doing so well, from the excellent Our World in Data. Explore it before thinking of any holidays abroad!
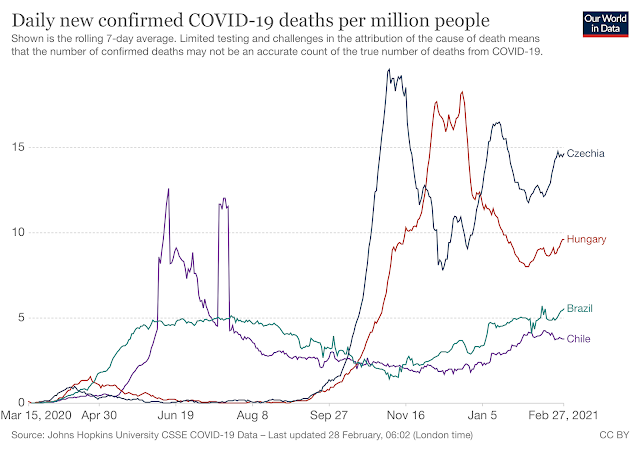
Nations not doing so well….
While looking at these graphs over the last year, I wished for a crystal ball to see how we would looked back on the whole experience. Perhaps this is it. Perhaps it’s not. Looking for a precedent takes us back to over a hundred years ago and the Spanish Flu.
How Pandemics end.
I will shortly write on the biggest pandemic of the century, Spanish Flu. The modern tools of epidemiology and virology means this is only now is being properly understood.
I have to say, for the sake of accuracy, that the H1N1 strain responsible for the pandemic did not come from Spain. It was first publicised there as there was no wartime blackout on pandemic news in Spain. Elsewhere it seems not causing fear and panic came before saving peoples lives. The graph below describes its three waves.

The H1N1 pandemic played out differently in different parts of the world and is estimated to have killed 50-100 million people. Most of these deaths were in the 20-40 age group who happened to have little resistance to that influenza strain. It was a different experience at a different time. This time, we’ve been lucky in this respect.
So even without vaccination, Influenza also came along in three waves, then receded to return on a seasonal basis and with intermittent novel strains causing pandemics. This is expected to be the future for our relationship with Sars-Cov2. A model for COVID19/21/22/23? It looks likely.
Pandemics end when the viruses have nowhere else to go. For Spanish flu, most of the world was infected, so deaths were high, for COVID we might have a long way to go before it runs it immunological dead ends – though uncertainties exist about how far we might be from that.
Moves are afoot to combine flu and coronavirus vaccines into one nasal spray, or capsule which would make the whole thing more acceptable and manageable. Technology to the rescue once again.
Vaccination update

new viral particles
I’ve had my vaccination and have, like most of us, accepted the Astra Zeneca viral vector vaccine. There is now good evidence that the 12 week gap till my next one does not reduce, and indeed might even improve the overall effectiveness.
Israel were the first off the vaccine blocks and have announced early benefits from vaccination in the elderly, with big reductions in infections even after the first dose of their Pfizer jabs.
This has been backed up by encouraging results suggesting that transmission is reduced also which will mean those who are vaccinated are effectively helping others as well as themselves.
Efficacy is measured in controlled clinical trials and when it comes to drug treatment, the hype generated by carefully controlled trial conditions doesn’t play out in drug effectiveness in the more complex real world. With vaccines it seems the other way around – they all seem better than we thought at reducing transmission, preventing illness and protecting against severe disease and death.
Comparing the risk of hospitalisation of vaccinated to unvaccinated people in an impressive Scottish audit revealed effectiveness of 85% for the Pfizer vaccine and 94% for the Astra Zeneca shot, though some uncertainties remain.
This has now been confirmed in England and Wales where vaccination has cut the risk of hospital admission of elderly COVID by 80%.
While vaccination is a big achievement, it is not the whole story, we will have to continue to take measure to reduce its spread and already the wearing of masks is now being referred to as reasonable ‘respiratory hygiene’ and likely to become far more common in the winter, as it has in Asia.
Johnson and Johnson have been approved by the FDA in America and do the job with a single jab, Novovax too will soon join the ever expanding collection. I’m sure that they are all in the process of thinking about boosters in the Autumn.
The success of the vaccination programme, delivered largely by the NHS, contrasts with the failure of the Testing and Tracing programme delivered by the private sector on top of a pyramid of unaccountable and even untraceable sub-contractors. This needs to be addressed and there are widespread calls for public health and the NHS to be at the centre of FTTIS (Finding, Testing, Tracing, Isolation Support), but will the Conservatives be able to admit they got this wrong? Humility is not their strong point, particularly when basking in the glory of the vaccination programme which has largely been the achievement of others. Such is politics!
This might come back to bite though. Without an efficient and effective testing and tracing system we remain vulnerable to future outbreaks and the further waves potentially forming out there in the ocean, waiting to crash on our shores.
Hesitancy on the wane?
Vaccination uptake in the UK is very high and despite some hesitancy, testifies to the success of a voluntary programme and perhaps the pitfalls of making vaccination mandatory.
That is not to say there will not be problems. For the unvaccinated, there will be no travel to nations that decide against entry – France, the USA and Australia come to mind. There will be new questions for individuals and employers of those who do not want to have the vaccine, so ethical issues a plenty. However, rates of hesitancy seem to be falling as shown by the results of international polling:
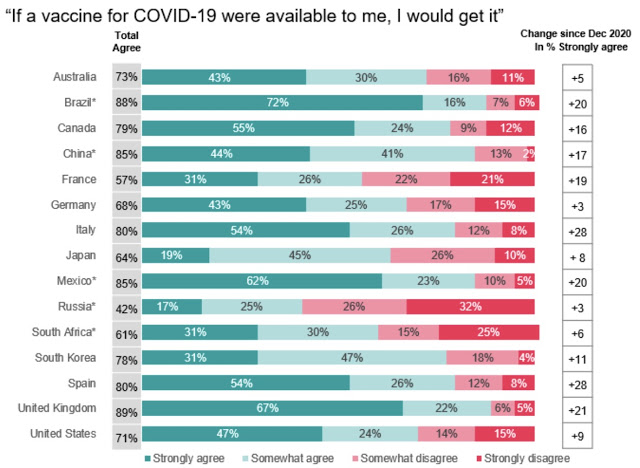
Thanks to Susan Levenstein for the graphs
There is already research looking at making oral vaccines and combining them with influenza for a one hit winter protection of viruses which will be with us for ever. The global community will have to work out how thorny issues of affordability, equity and access. Perhaps COVAX will show the way.
Variant watch
Sars-Cov2 makes a couple of mutations a month, low for a virus thanks to its genetic spellchecker. That number is directly related to the number of viruses replicating, so the greater the number of cases, the more new versions there will be, with adjustments made to improve its ability to spread by stronger binding to our cells and escape from our immunity and vaccines. We might regret not having taken a more ‘whole world’ approach to vaccination.

There have been two recent change of note. The N501Y change has flipped a couple of bases on the receptor binding domain of the virus. N and Y are codes for the amino acid and 501 refers to their position on the spike protein. The effect of this is to exchange a negative charge for a positive one and rather like a tiny magnet, makes it stick better to our ACE2 receptors.
The E484K mutation likewise sticks better to our cell receptors, but also means that antibodies also stick to it less well. It is thus better at escaping our own or our vaccine induced defences.
The P1 variant from Brazil contains both of these and has arrived at our UK shores a week before sluggish quarantine measures were put in place – rather like a para-medic turning up late for a cardiac emergency on a pushbike. To then have lost one of those infected with P1 due to an error in form filling shows both how far we have to go and that we are not out of the woods yet.
How this will play out now is uncertain, but our vaccines do not work so well against this latest model of COVID19. Somewhere out there is an individual, recently returned from Brazil, infected with P1 and unknown to public health bodies. Lets hope that person is not one of the small number of people who are effective super-spreaders.
Might this be the next pandemic chapter? It wont be long before we know.
A New Year.
Like 2020, this year is going to be very different from normal, if ever there was a ‘normal’ year. We are not out of the COVID woods yet, but while there are good grounds for optimism, there are some for pessimism too. In the middle somewhere is reality and how it will play out.
For all or us there are now questions of how we pay back the £271bn the pandemic is said to have cost the Economy. For perspective that is equivalent to £9,700 per household in the UK.
One of the reasons we have done so badly is our low level of ITU beds. These beds are just one tiny cog in the vast machinery of our civilisation, but the pandemic has shown how it is critical to how society works when face with a health crisis.
We have 7.3 per 100,000 people, while the US and Germany have more than 30, more than four times our capacity. We have found to our cost that skimping on provision of ITU beds, partially at least driven by austerity costs money – lots of it. We also have found that poverty and poor public health are unaffordable.
It also comes at a time when we need to reconfigure humanity for the challenges of our times which in our collective vision lack the urgency of the pandemic, but which are looming far larger in terms of impact on all our lives. I have thought long and hard about how to improve outcome for people with MS as well as other illnesses, and it it crystal clear the major threat to our future is our destruction of the foundation of our existence – the oceans, rivers, land and the atmosphere.
There are enough financial resources in the world to address these problems, but much of what is spare is simply in the wrong place – those trillions in the hands of a small number of people somehow has to be mobilised for the greater good.
Further, as I examine my day to day life, I reflect on the luxuries which in good part led to the pandemic. Freedom to drive and fly anywhere and anytime we want. Freedom to buy whatever we can afford from wherever it comes. Freedom to use as much energy as we want. All of our freedoms depend on how much we earn or own, and the availability of resources.
A good friend advised of the conflict between the social animal we are and the individual we have been encouraged to become. Collective thinking will mean that perhaps the age of Freedom will give way to the age of Responsibility and Consequences.
Times are changing fast.