It’s 75 years ago since healthcare was transformed in this country. In a war weary country there was not only a thirst for something better than what went before – hence the Labour landslide – but a need to deliver rapidly evolving medical advances to everybody, irrespective of income.
Since then the NHS has been a shining light of what can be done to deliver healthcare free at the point of delivery. How is it faring at 75?
The NHS still does amazing things, every single day and continues to ensure that huge numbers of people are correctly treated at the right time. The graph below shows how UK life expectancy has changed, with big improvements either side of the inception of the NHS.

Life expectancy improvements in the UK. It is now levelling of, and for the socially deprived, falling. In 1952, the UK was 7th in the world, now we are 36th.
Of course, much improvement was made due to measures taken outside healthcare, but better care of children has made a big impact and the cradle to grave health services have played a huge part too. Many new and effective treatments are available and care for my own MS has been transformed from a no hope diagnosis, to one where effective treatments and monitoring are now routine.
I look back on my time as a GP with affection and gratitude, and as a patient I have been well served. Nevertheless, there are glaring, growing problems and it’s clear that unless there is a significant change in direction the NHS will be unrecognisable in a few years. Over my career it has been transformed and it will be transformed again. There are many claims of its failure, but was does this mean?
What does failure look like?
How does a health system fail? It isn’t a matter of a single event – there will be no “Closed” sign on hospital doors – but a process of steady incremental decline. Terminal markers being, for instance, poor outcomes from cancer, long waiting lists and junior and now even senior doctors and nurses going on strike because they live and work in the NHS, can see exactly what is going on and have had enough. Too may staff can no longer cope and are taking the option of final resort and leaving.
The number of doctors and nurses in the UK had already been allowed to drop over the years as the table below shows. Bed numbers have tumbled too.
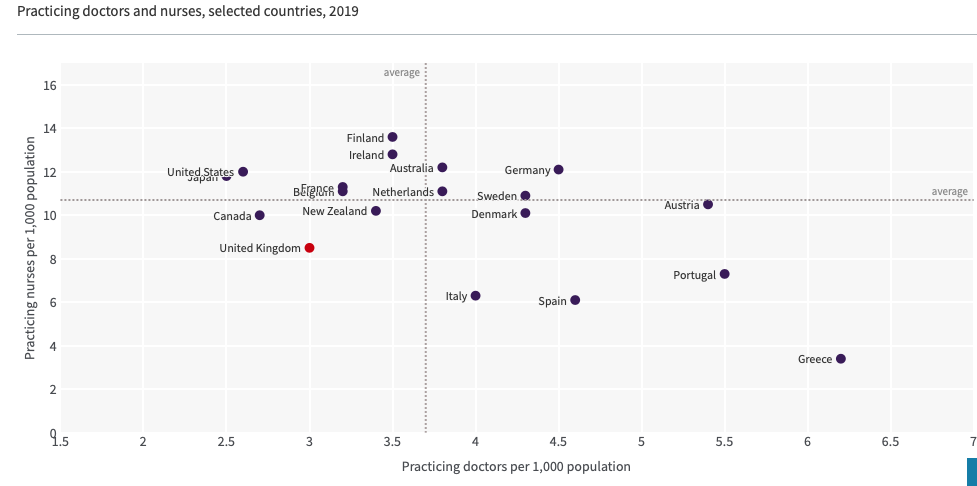
Not where we want to be….
We all see this in the news, but it only hits home when individuals are failed by delays which make treatment more expensive and less effective. Frustrating for all, deadly for some.
A telling example
A short personal story of my trip to A+E with a friend in need of urgent assessment revealed much. A caveat was that my visit followed a bank holiday weekend, but bank holidays are not some sort of surprise disaster which befalls us – they are in the calendar. Yet as the ambulance rolled into A+E, an unexpected calamity was impression I was faced with.
There were 22 ambulances stacked up outside A+E, each containing patients in various stages of need. Some had intravenous infusions, some being given oxygen, many looked ill. In addition to usual A+E loading bays, a whole new car park had been commandeered for queuing ambulances. In other words this was not exceptional.
The professional and helpful ambulance crew told me more. Some of their shifts are spent entirely in their parked ambulances outside A+E! This not only means deadly delays for patients in the ambulances, but some really tragic losses occur when ambulances don’t reach people quickly enough due to the fact that so many are out of use, parked. Waiting.
In my chums case, blood tests were taken fairly quickly in the RAT area (Rapid Assessment and Treatment) and four hours later the results were found to be within normal limits. The A+E consultant (who was in effect doing a ward round in the car park) informed us the wait for a cubicle in A+E would be a further four hours and there were people in cubicles as we spoke who have waited for a ward bed for a further three days.
Harms
The harm to wait this long for an assessment outweighed the benefits of further urgent assessment so we went home with my ambulant chum in a taxi to get the community teams to urgently address the ongoing issues. An eye opening experience.
COVID has played a big part in this, but it was worsening before the pandemic. One estimate calculated that in 2020-21, 4500 excess deaths were due to prolonged waits in A+E. That is on the back of the 500 annual deaths due to delay in the arrival of an ambulance after an emergency call. The ambulance crew looking after us told me that they personally knew of deaths caused by inability to get ambulances on the road quickly enough.
Clogged
Poor social care is the ‘blockage in the pipe’ upstream, meaning it’s impossible to free up the desperately needed hospital beds. Brexit has made matters worse. Poor pay and low investment in the care sector is a big part of the problem and reveals a serious lack of capacity and investment, a can forever kicked into the long grass by politicians.
Primary Care
Primary care too is in trouble too, particularly in our towns and cities. My old practice was not alone in finding it impossible to recruit new young partners and had to hand its contract back to the NHS as they could no longer offer a safe service. That surgery now follows the new model of sessional and locum doctors which means that doctor-patient bond, so fundamental to good care, is becoming a rarity. When you see a different doctor every time you need help, it means the GP doesn’t know you either and has to start from scratch.
The future
It’s more important than ever to do our best to stay healthy, though this is not always easy and often downright impossible. Your can’t change your genes. It’s hard to escape poverty, to avoid financial stress, not to live in a polluted environment, to eat, and sometimes even find good food, be well educated and to make good decisions. Much of our health outcomes is beyond our own individual choices, however important they are.
For those who need the care of last resort, which an ambulance call so frequently, it’s a roll of the dice.
With ongoing privatisation, the development and rollout of AI, new technologies and treatments as well as new threats to health, our experience of healthcare will continue to change. The staffing crisis which will not soon be addressed unless pay and conditions are improved. The recent workforce plan, though welcome, seems to be far too much dumbing down to me not going to address current problems for some time.
As I have said before, Conservatism, that emphasis on shrinking the public sector reducing taxes is creating harm. Brexit which put party before country, the folly of austerity, and ongoing poor government is bad for health and will take some decades to overcome, if we ever do.