 |
| Sars-Cov2-19 |
One of the few benefits of the pandemic for me has been my introduction to new methods of on-line learning and the expanding world of Webinars.
They might lack the personal touch of old fashioned meetings, but are good in so many other ways. No climate busting travel, no expenses, amazing ease of access – and no-one sneezing over you!
I have listened, student like once again, to speakers from the world of immunology and MS discussing COVID19, virology, vaccination, immunity – all subjects close to my heart. This is my report back.
Fighting infection –
Our defences
As ever with immunology, descriptions of our natural defences against pathological invaders causes me to sit back in amazement and wonder! I’m not one for military metaphors, but it really is a battle between our immune system and the outside world with our white cells on the front line.
The very fact that you are reading this means you have overcome countless infections which have been dealt with by your defences. Bacteria, fungi, and viruses have to be highly specialised to overcome the obstacles put in their way. They are expelled by the mucus of a runny nose, inhibited by fever, hit by numerous biological weapons as they try to gain entry. Then they come up against the white blood cells.
.
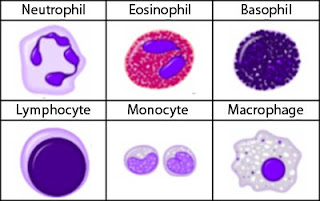 |
| Our wonderful white blood cells |
I won’t go into the mind-boggling details in this post (I will later) but suffice it to say for now that there are two phases to our reactions to COVID once they gain entry.
First, some of our white blood cells (right) behave rather like millions of micro-police officers (neutrophils and macrophages) who float around the blood looking for trouble, bashing trouble makers with their basic readily available equipment and the aggressive natural “Killer T-cells”.
After that, they call up “back-up”.
This is provided by lymphocytes and the others located in their ‘stations’ in the spleen and lymph-nodes. When called up, they work out who invaders are and if they have come across them before. Then specialised teams can deal with known culprits and process the details of those they haven’t. New units of these lymphocytes are created to clobber invaders with some pretty impressive immunological weaponry specifically designed for each individual foe. As with severe COVID, they sometimes cause mayhem in the process, called the ‘Cytokine Storm”.
The reality of our immune defence to COIVD19 or any other pathogen is many times more complicated than any labyrinthine intelligence service, so the analogy ends there. Apologies to any immunology savvy readers who might gasp as this over-simplification.
Yet that is the essence of our response to COVID19.
Vaccination
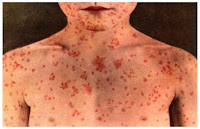 |
| Measles |
Vaccination is our attempt to get our immunological defences ready for the known culprits in our infection prone modern world, and was much discussed in the Webinars. Its recent achievements have recently been brought into sharp focus with the upsurge of measles following the Wakefield scandal; there were less than 50 UK cases of measles in 2003 before the scare and by 2009 the rate climbed to 1500.
Indeed, the history of the world was changed by the BCG vaccine against TB termed “The Greatest Story Never Told” by one author. I am glad of the fact that so few of us doctors have ever seen a case of Diphtheria or Tetanus. I have never had to diagnose Polio though met quite a few who were disabled by this infection in their youth. I don’t need much convincing as to the benefits of vaccination.
On to 2020 and much hope is naturally focused on a vaccine to COVID19, but first a further word on why this virus is such a problem and in particular why is it so infective?
Infectivity of COVID-19
You might be aware, indeed sick of hearing about the R0 number. It stands for the Reproduction rate observed in susceptible populations. An R number less than one and the pandemic fizzles out.
 |
| What a sneeze can do. |
COVID19 is highly infectious with its Ro number about 3. This compares to Ro numbers for measles of 13 and the savage 1919 flu outbreak of 2. Its main mode of transmission comes from people without symptoms shedding and share viruses. Travellers and others who meet lots of other people before isolating are termed super-spreaders.
The R number will fall as more people become immune either by getting the infection or by vaccination, then it becomes harder for the virus to find people with no antibodies which neutralise it..
Looking at it another way, human being’s Ro number (called our fertility rate) is currently 2.4 with obvious resultant global over-population. Humans and COVID19 both spread very rapidly.
Humans – the ultimate super spreaders
And therefore, in this modern hyper-mobile world:
Unless that is, we do something. So how do we defend ourselves?
Our own immunity to COVID-19
Antibodies to COVID19.
 |
| Antibodies (in red) hitting their target |
After initial uncertainly it now looks like we do develop immunity after infection with COVID19.
An early Chinese study 0f 170 hospitalised patients found antibodies in 100% of cases two weeks after infection. More recently researchers in Paris found 98% of hospital staff who had mild infections developed antibodies, when measured 40 days after the infection. Only one case out of 160 failed to do so.
While much uncertainty exists about how long this lasts, this is good news. It means that antibody tests are useful at least over that timeframe and that immunity seems widespread after the infection.
What can we learn from SARS-Cov in 2003?
This was a similar ‘sister’ coronavirus responsible for the SARS outbreak in 2003. It was more severe, but less transmissible. Neutralising antibodies which protect against re-infection with SARS were found to last up to three years after infection, then declining.
If this happens with COVID19 it will be good news, but again right now we don’t know for sure. Tracking antibody levels from blood or saliva tests with time will be give us more definite answers.
Might immunity against other coronaviruses help?
Coronaviruses have been around for some time causing a range of milder illnesses such as colds and croup. It would be helpful is there was some cross-immunity against COVID19.
It seems that 30% of COVID negative blood donors were found to have some white cells which target the notorious spike protein, though at lower levels than those who had COVID19 infections and less completely too. This is really interesting and perhaps offers some hope that some of us at least have some anti-COVID19 weaponry already installed.
As ever the authors are cautions, rightly so, it is however, very interesting indeed.
Hello herd immunity?
So is it a two horse race between the development of a vaccine and the acquisition of herd immunity through infection?
So what does herd immunity mean?
Then they just wont to be able to spread from person to person. End of pandemic! How far down this road are we ?
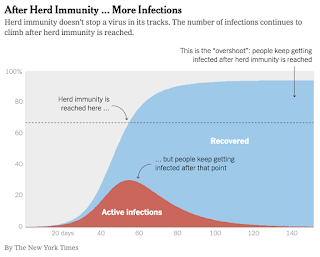 |
| Herd immunity |
The WHO have stated that any policy aimed at getting to herd immunity is dangerous, and looking at levels of immunity in the human herd so far, I certainly see why.
Lockdown lottery.
Sweden is a very different place from the UK, it is a huge country with a sparse well educated population of 10 million people and far less health damaging social inequality than here.
They have taken a different approach to managing the epidemic, relying on social distancing, with a more far more lenient unenforced lockdown. They felt their approach was best for them without explicitly aiming for herd immunity.
Predictably they have had more initial infections with a higher mortality rate. Like in the UK, this has been particularly severe in neglected care homes.
So is Vaccination the knight in shining armour?
Vaccination to the rescue?
 |
| A chunk of RNA |
then vaccines developed with more tried and tested methods will be available later next year or early in 2022.
Us old owls tend to fight infections less well. For the same reasons, we develop less of the protective antibodies the vaccine are intended to stimulate. Given the single biggest risk factor we have is our age, even a successful vaccine vaccine is therefore no panacea
Issues of global coverage of the vaccine in this global age also loom large. As I said earlier, outbreaks anywhere = outbreaks everywhere, so poor nations are going to need access to vaccines to help control the pandemic.
Yet if the challenges can be overcome and the problems of manufacture, delivery and administration are sorted, then a successful vaccine will accelerate our march to herd immunity and the end of the pandemic.
Might we be lucky and COVID19 mutate into something less unfriendly?
Mutant COVID heroes??
 |
| Less unfriendly Sars-Cov2-19? |
There was a bit of good news. Viruses do mutate, changing aspects of their proteins from time to time as they reproduce, rather akin to changing their clothes.
In general terms more severe strains cause more severe illnesses, and so people with the severe strains tend to stay in and isolate more effectively. This means there is an evolutionary pressure on milder strains to spread more widely and generate immunity without so much suffering. This too would help the pandemic to peter out. Perhaps.
This was evident early in the pandemic in China. they isolated two strains, one far more severe initially accounting for 70% of cases, but falling in frequency as early as January as the less severe spread spread more rapidly.
However since then few significant mutations have been reported so Im not holding my breath, even if I am crossing my fingers.
Conclusion – The anti-pandemic recipe
After all that, I am left with perfectly understandable feelings of uncertainty. However is it not a horse race between competing approaches and perhaps it will be a little bit of everything that ends the pandemic:
- Suppression of the viruses ability to spread with testing, tracing and local lockdowns
- The summer season reducing infectivity(at least in the north)
- Increasing levels of our own immunity to COVID19
- A lucky mutation or two.
- Vaccination.
- Time
Two other things would make a big difference, and they, dare I say it….. a healthier leaner fitter population and better leadership. We really have made a dogs dinner of things so far (more on this later) and so continue with levels of infection which might well make another wave or two inevitable.
So, while waiting for pandemic history to be written, I’ll say it again……. use the summer to get fit for COVID19 – just in case.
