Much has happened since my last post on COVID in our care homes, just a few long weeks ago. At that time I was worried about the viability of care homes at all in the face of the mortality affecting their residents; thankfully the government had come up with more cash (£2.5bn) to plug the holes, but like in other sectors, there are many cans being kicked down the road.
Care home deaths
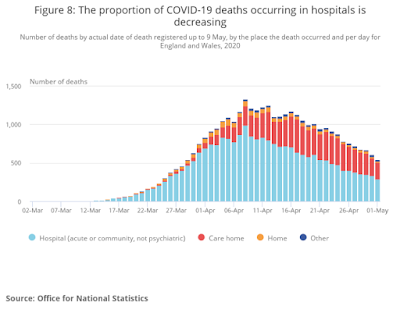
In the UK nearly 10,000 residents of care homes have died with COVID on the death certificate, though the real number is likely to be higher due to the problems faced by doctors trying to certify the cause of death without test results. Early in the pandemic this was well reported.
Professor Sir David Spiegelhalter, chair of the Winton Centre for Risk and Evidence Communication at the University of Cambridge: “I was genuinely shocked to see the spike in deaths and almost half the spike in deaths did not have Covid-19 on the death certificate. That could point to a huge under-reporting of deaths at home and in care homes”
Added to this, some residents of care homes are dying in their sleep. I have listened to two medical chums who have told me of many peaceful nocturnal deaths. The victims of COVID were frequently unwell one evening, to be found dead the next morning. This fits with the notion that oxygen saturation levels can be very low in patients who don’t feel that unwell.
In the past I used to increasingly put the cause of death on death certificates as “Old Age” which often best reflected reality. It seemed more respectful than fishing around for a diagnosis which often wasn’t clear on, in this case, available from test results. The inevitable conclusion is that deaths from COVID in the care sector are underreported.
Indeed this could be a significant under-estimation. Number cruncher’s at the London School of Economics estimate that if the deaths of other care home residents are taken into account, as well as some of the deaths of care home residents counted in hospital, the number could be as high as 22,000.
Care homes are a neglected part of the front line.
Care home staff
Many members of staff have been infected and some have died. ONS report:
“The rate of COVID-19 deaths among male social care workers was 23.4 deaths per 100,000 men, compared with 9.9 deaths per 100,000 for the male population. The respective rates for females were 9.6 and 5.2 deaths per 100,000 women”.
This is hardly surprising in that many COVID positive patients have been discharged from hospitals to poorly prepared care homes equipped with very poor protective equipment. For me this is the worst case scenario when it comes to planning.
COVID infections in care homes are, even with the best equipment, very difficult to contain, particularly when air conditioned.
Although the decline in deaths has been slower than hoped, the lockdown has achieved its stated aim of managing the initial phase of the pandemic without overwhelming NHS services, the question is what to do now? This question is critical in the care home sector.
Locally
Here in Plymouth the pandemic has been slow to bite due to restrictions in travel from more affected areas. I called a couple of care homes I used to visit, one nursing, one residential to see how they were getting on.
They both have so far had no COVID patients and indeed will not take anyone suspected of COVID as they are maintaining their COVID free status. They are pre-COVID. They have invested in and are using PPE bought in early in the pandemic and are thus shielding their patients from potential infections from the staff. They have done an amazing job!
The nursing home have even had volunteers on furlough coming in to help with relevant non nursing tasks. People really can be wonderful!
In this particular residential home, effective lockdown was started before the Government announced it and they have supplied their own PPE. Relatives are able to visit with relevant PPE and distancing and residents can go on assisted walks only up and down the quiet road outside. Co-operation has been outstanding. Again any potential admissions will have to tested to ensure their COVID free status.
So far so good for these two homes. The lockdown has prevented the spread of the virus from the wider outbreaks in London and elsewhere, and they have, pretty much off their own backs kept themselves free of COVID so far. They both are aware that COVID is still very much around and that there will be more cases.
So how can we continue their success?
Solutions
Breaking routes of transmission.
Hospital discharge of elderly patients recovering from COVID is a fundamental problem. More so in the elderly who can continue to have viral material present in nasal swabs for up to a month after the onset of symptoms. So, even after the illness seems to have settled, they need to be seen as infective until they have had two negative nasal swabs or failing that, a month has passed from the onset of symptoms.
They should not be re-admitted to their care homes of origin until that takes place. This is the only way for homes to continue to care for their 400,000 residents. Frequent testing and PPE will continue to be needed to prevent the 1.3 million staff looking after them from spreading infections in the homes.
So until viral shedding stops, care home patients will have to be either kept in hospital and be insultingly labelled as “bed-blockers” or discharged to any adequate form of intermediate care ensuring ongoing quarantine.
Perhaps the now idle Nightingale hospitals could be re-purposed for the management of recovering COVID patients until they have stopped shedding the virus. PPE and rehabilitation services could be concentrated in these areas and discharged patients with negative nasal swabs would thus pose far less, or no risk back to their own care home.
If the big Nightingale hospitals are not suited for this task, specific specialised nursing centres could be established in re-purposed local facilities for this well defined role, again with the right equipment and staffing levels. Testing would determine when patients are safe to discharge to the usual care home.
Make the most of local skills and knowledge
There are major concerns regarding the vastly over-centralised methods the Government are embracing. New sparkling Apps and contracts for the private sector are pretty much ignoring local primary and public health teams who would be well placed to identify cases and deal with any outbreaks. Care establishments, of any type should have priority for teams of tracers and testers as containment in the wider community seems now to be a distant pipe-dream, a political fantasy.
I was made aware of how things can go wrong if local expertise is not employed. In Plymouth a local hotel was repurposed for recovering from COVID, but was sadly found to be unsuitable for patients in wheelchairs due to narrow corridors and so proved unsuitable for the job. Admissions so far – 6.
Another example of the difficulties of top down planning was a recent directive to care home owners to ensure that doors to residents rooms were fitted with letter boxes, to make them feel at home. Good idea it might seem, until fed back that the doors were fire doors and making big holes in them might not be a good idea. Letter box ideas quickly dropped!
The over centralisation of our public sectors is being show to be dangerously inadequate. There are ways of using the knoweledge of those on the ground to not make mistakes, and at this point, planning for next winter we need to get the care sector working well.
Advance personal planning
Any person is a care home, or many who are not, who do not want intensive care, should make their feeling know in a living will and advanced directives. These should be discussed with your family, with staff and communicated to the GP so it is clear what is expected should the need arise.
The staff.
First and foremost, the staff have to be cared for. Heartfelt clapping every Thursday is well received but the ability to carry on their job without spreading the illness within and without the care home is vital to get right as soon as possible in preparation for next winter.
The backdrop to this is worrying. The turnover rates of care staff are high for good reasons, It’s hard, low paid, demanding and now dangerous work. Would you do that for £8 an hour?
Despite that, through my career I have been so impressed by the dedication of care home staff. I have seen skilled care at its most inspiring in care homes in Plymouth. There have been many extra miles walked by many members of staff. They have been societies unsung heroes for too long!
COVID is re-ordering our priorities and not before time, those caring for our health and looking after us in our infirmity need recruiting, resourcing and rewarding. It needs to be seen for the noble career path it is with built in opportunities for learning and training.
The next phase
Of course, we all hope there will not be another wave, that the first phase will be the last, but I cant help but feel this is vastly over optimistic. COVID has not gone away.
The big concern is the winter. Another wave then could well be more severe, and we have to do far better than we have done in the first, where advanced planning for the crisis was left to care homes themselves.
Some significant advance planning has already been done to prepare care homes for flu epidemics, but its relevance to COVID was either not recognised, or it seems, ignored.
Till now, we have spread the virus from where it was concentrated, in hospitals, to care homes where initially at least, it was absent. From there COVID can of course, be spread out from the staff into the wider community. The Genie flew out of the bottle and scarpered!
Hospitals, care homes, isolation hospitals or adequately repurposed facilities looking after their defined caseloads, backed up with prompt local testing tracing would be likely to ensure that the inevitable multiple outbreaks this summer or worse, next winter, will be able to be extinguished before they become out of control and out of our hands.