It doesn’t seem to prevent COVID19.
Since starting this blog, Ive written a number of posts on the benefits of Vitamin D and how we are generally not making enough of it due to our indoor lives, fully clothed habits, poor diet and excessive use of sunscreens. In terms of preventing COVID19, the biological case and observational evidence for taking Vitamin D seemed good. It is also clear that low levels of the vitamin are associated with poor outcomes. Certainly in the precautionary sense, supplementing with Vitamin D which is cheap, safe and likely to do good in other ways seemed a good move.
Yet in terms of preventing COVID19, it seems I was wrong.
CORONAVIT trial
The recent CORONAVIT trial showed pretty clearly that taking supplement of Vitamin D made little difference to how many people went on to become infected with COVID19. The authors conclude:
“Among adults with a high baseline prevalence of vitamin D insufficiency, implementation of a test-and-treat approach to vitamin D replacement did not reduce risk of all-cause Acute Respiratory Infections or Covid-19.”
This was a trial performed by a team who have been keen on Vitamin D in the past and who recently published a meta-analysis of trials for Vitamin D which showed a small but significant benefit of taking Vitamin D on respiratory infections, so any notion that they are biased against simple cheap treatment doesn’t hold up.
The trial looked at 6,200 people, half of whom were randomly invited to prick their finger to get a Vitamin D level. The aim was to treat those with levels below 75nmmol/l with either 3,200iu daily, a high dose, or 800iu daily, which is more like the dose recommended for bone protection. Outcomes were compared to the other half of trial participants who were not tested or treated. Of those offered testing, 95% accepted and 87% of those were treated as their levels were below the 75nmmol/l. Here’s what happened…
76 (5.0%) people in the high dose group, 87 (5.7%) in the low dose group and 136 (4.6%) in the no treatment group went on to test positive for COVID19. In other words, there was no difference, even though they selected for treatment those with known low levels of Vitamin D, and in those people Vitamin D levels increased to acceptable levels in the blood.
The study has some limitations. It doesn’t look at people with profoundly low levels of Vitamin D who may benefit more, nor did it look at severity of disease (that would need a much larger trial), and it didn’t measure Vitamin D levels in the control group. Nonetheless the results seem disappointingly clear and join others which have shown little benefit in terms of treating the acute illness with Vitamin D.
So there we go. I was wrong. Foe me, this means the Vitamin D story just got a lot more interesting.
The impressive evidence of the link between low Vit D levels and the incidence of various illnesses, including MS and many infections along with COVID19 is robust. So why do people with low levels of Vitamin D do badly? In other words, why does low Vitamin D predict but not prevent a poor outcome?
There is further light to shine on this. Literally.
The Vitamin D paradox
I am naturally suspicious of supplements. To imagine that a simply supplement can right the wrongs of genetics, lifestyle, or luck is usually wishful thinking for the consumer and commercial opportunism for those wishing to cash in. Billions have been extracted from shallow pockets, the vast majority of which could have been better spent on better food or something more positive than what is usually a useless pill or potion.

Polypharmacy, too many prescribed medicines, is a real problem – but so too is taking too many needless supplements.
The idea that a simple supplement of Vitamin D is a cure all is confounded by the following four big reasons:
For one thing, low Vitamin D levels mark more than lack of sun exposure. They are associated with indoor work, sedentary lifestyle, poor diet, poverty, unhealthy living environments, and being too unwell to get out and about – all of which cause illness independently. These underlying issues are not corrected by supplementation.
Secondly, Vitamin D levels are lower in people with dark skin. First and subsequent generations of immigrants have increased health problems and racism, with all its health consequences and costs, is sadly alive and well. Again, these factors won’t be changed by a simple supplement even if the case for supplementation to avoid Rickets and osteoporosis in those with low levels is compelling. It still makes precautionary sense for anyone with a dark skin living in temperate climes to take Vitamin D, but is far from the whole story.
Then there is the fact that being ill with inflammatory disorders and infection depletes Vitamin D and so low levels are to some degree caused by active illness – this is called reverse causation.
Finally, there is more to sunlight than meets the eye. Perhaps it has other effects? So low sun exposure leads to low Vitamin D levels – and sure enough low Vitamin D levels are associated with infections and poor outcome – but simply taking Vitamin D to get your levels back to normal does not work. Might the answer lie in other beneficial effects of sunlight?
Shining a light on sunshine
Sunlight comprises more than the UVB we need to synthesise Vitamin D. While you need UVB to make Vitamin D, visible light and Near Infra Red also have their biological effects. Exposure to sunlight has a significant effect on increasing mood enhancing Serotonin activity in the brain and its lack may well be at least in part, responsible for low mood in the winter.
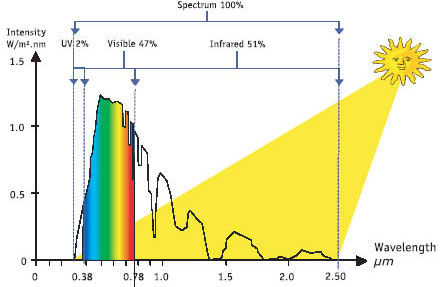
There is more to sunlight than meets the eye – we only see what our vision allows us, visible light.
The results of the CORONAVIT trial hints that there is some other benefit from sunlight exposure beyond Vitamin D we are not aware of. It is certain that there is much we don’t know about the action of sunlight and it may be that time outdoors provides all sorts of interacting and synergistic benefits. However, another important intracellular hormone is emerging as important.
Might some of the benefits of sunlight be due to melatonin?
Melatonin
This potent free radical scavenger and antioxidant is manufactured within the mitochondria of our cells due to the action of Near Infra Red (NIR) light which comes from wavelengths the opposite side of visible light to UVB and is invisible to the human eye.

MELATONIN – another hormone influenced by light.
So Melatonin is another vital element of the body’s continual efforts to maintain an even balance within every cell we have, something called “homeostasis“. (from the Latin ‘keeping things the same’). It is a free radical scavenger and antioxidant produced within the mitochondria of cells under the influence of NIR. This is in addition to the production of Melatonin by the Pineal gland which is so important for circadian rhythm and sleep.
NIR penetrates though clothes and deeper into the skin than UVB and is present in any form of outdoor light. So unlike UVB and Vitamin D, it doesn’t have to be sunny for it to stimulate the manufacture of melatonin.

NIR penetrated further into our bodies than UV or visible light.
We are also getting less of it than we used to. NIR used to be able to penetrate old style windows and was emitted from incandescent lights. Now we have glass designed, rightly for energy efficiency which keeps NIR, and often UVB out and LED’s are great at emitting light in the visible part of the spectrum, but no NIR at all.
This interesting research shows how exposure to NIR has declined as we develop glass and indoor lighting technology to address the needs to conserve energy.

This is another way we are being depleted of what we need from the sun and might answer the paradox of why low vitamin D levels are associated with many illnesses, but simply taking Vitamin D supplements does not work for cancer or COVID19.
To summarise, the pic below shows what we currently know about the effect of sunlight on our physiology.

A trial of sunlight?
We can perhaps, forget about trials for this. Randomising people to avoid natural light would be as ethical as randomising a set of trial participants to eat junk food. Do no harm, that overused, simplistic mantra belonging to ancient Greek doctors is applicable here. (The modern version might read – do more good than harm) This early study from Jakarta showed a significant association of sunlight exposure with COVID19 recovery.
Should we redesign glass which would let NIR in but be less efficient in terms of insulation? No. Or go back to NIR emitting but power hungry lights? No. Again, we have to cut down drastically on energy use to have any chance of survival, and soon. So what to do?
Sun exposure is good.
The complex science, the trials, controversies and arguments boil down to one simple thing. Get outside and into the light on sunny days, on cloudy days, on any day at all. Open the window if you can, and get out of the shade whenever possible. Who knows what more we might discover about sunlight? Perhaps intracellular Melatonin is, like Vitamin D, a marker of some other effect yet to be discovered? Sunlight exposure will take care of them all.
That has to be the bottom line, and far more important than we might have thought.

This may have made a good deal more sense than we thought. Sunlight for people recovering from TB in the USA.
Don’t stop taking Vitamin D
Meanwhile I, along with just about everyone else with MS, will continue to take daily Vitamin D. The recent VITAL trial showed that it reduced the incidence of autoimmune illness by 22% which is highly significant. The researchers conclude:
“Vitamin D supplementation for five years, with or without omega 3 fatty acids, reduced autoimmune disease by 22%, while omega 3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant). Both treatment arms showed larger effects than the reference arm (vitamin D placebo and omega 3 fatty acid placebo)”
For people with autoimmune problems taking it also makes sense. This is due to the striking increase in incidence with increasing latitude and decreasing sun exposure, and its significant association with poor outcomes.
Anyone who works indoors, commutes by car and has indoor interests might well be better served by changing lifestyle and taking Vitamin D supplements as a substitute for some of the benefits of sun exposure when this is not possible. There is no escaping the conclusion that sunlight is better.
Don’t start taking Melatonin
What about taking Melatonin? It is currently licensed and available on the NHS for short term sleep problems and treatment of jet lag, but treatment for other benefits is uncertain.
Some can be obtained from the diet. In a Japanese study, a small but significant association was found between dietary intake and longevity. Melatonin is present in many foods including cherries, goji berries, olives, and walnuts.
As melatonin seems to be manufactured within cells in response to NIR and then backed up by secretions from Pineal gland, simply gulping a dose and hoping to match the complex physiology going on within our internal system may be a bit quixotic, particularly as getting outside could do the job.
Sunlight and skin cancer
Sunburn has risks and so care continues to be needed with sun exposure and more so with the ozone depleted atmosphere. The common scenario of an indoor lifestyle, followed by a holiday trip to sun-drenched climes burns the skin and is the nightmare scenario for the risk of melanoma and other skin cancers. However, it also seems that safe sun exposure can also be associated with a better outcome for people with melanoma and, like with MS, those with sun related skin damage do better than those without.

The worst of all worlds?
What this means is that sunlight exposure is healthy and might even reduce the risk of melanoma, as long as you don’t get burnt.
Sunlight, including simply being outdoors, may be an awful lot better for your health than we thought.
Thanks for reading this post. If you have any comments of questions then do use the box below to share them, and in the meantime, close the door behind you and…….
