As Einstein so famously said, making mistakes is human, to repeat them, insane. We do things, learn lessons, repeat what we do well and not what we don’t. Ideally.
Scale that up and we have this years experience with COVID to look at. We have different nations and different ways of managing the virus to compare, so it’s time to scratch our heads and reflect. As ever, this is not easy. Humble pie is in the oven, cooking time uncertain.
Now that the data from COVID is piling in from all over the world, it’s clear that rates of infections in the northern hemisphere are falling, though globally the pandemic rages on. The NHS is reconfiguring again, this time to deal with the backlog of work built up over the first wave as well as people needing ongoing help with treatment and rehabilitation from COVID19.
So for us, perhaps that is the end of the beginning. Or is it?
Fattening curves.
Im afraid this isn’t a typo.
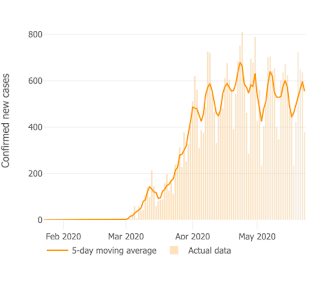
Here in the UK new cases seem to be running along at a stubborn 3,000 or so a day over here and deaths rates are slowly falling – our curves are flattening, but fattening too.
Looking wider, we have not flattened the national curve in the way in the way we might have hoped for when compared to our continental neighbours. Have a look at the information from John Hopkins University in the US is you want more details. Their level of detail is incredible.
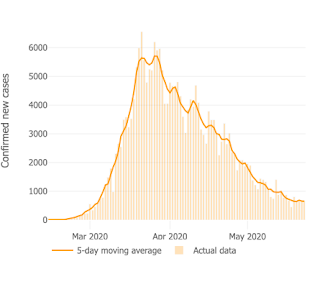
Here is our graph, with the decline in cases far slower than the increase in March.
 |
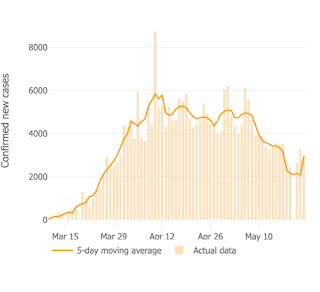
| Italy daily cases and 5 day average |
There are big differences within countries too, in London cases are now falling, elsewhere they are increasing. The need for regional and local management is looking increasingly essential to deal with potential summer outbreaks and winter waves as well as the endemic phase thereafter.
Spanners in the works:
I have included cartoons to make reading this section more bearable.
Austerity
The ongoing impacts of slimmed down public services mean that any theoretical savings made by austerity have been dwarfed by their costs. In other words, investment in the future works.
Our slimmed down local councils and public health bodies in particular have not been able to do the job they are designed for. Austerity was behind this, but also a politically driven centralising of power unheard of till now. Our council budgets have been cut to the bone, even before the crisis they were struggling to fund their legal obligations in care and welfare to our children.
Without a shadow of a doubt, austerity has cost lives, created misery and cost money.
Advanced planning.  Not because it wasn’t done, but because good planning has been ignored. I listened to Jeremy Hunt last night revealing his take on the problem with planning. It is not, he said, that many of the recommendations of planing exercises were not acted upon but that they were designed for a novel flu virus and not for coronaviruses.
Not because it wasn’t done, but because good planning has been ignored. I listened to Jeremy Hunt last night revealing his take on the problem with planning. It is not, he said, that many of the recommendations of planing exercises were not acted upon but that they were designed for a novel flu virus and not for coronaviruses.
This is unbelievably lame as we had already had warnings from SARS and MERS to alert us to the real dangers. Lack of sufficient PPE in the stores tell the story. Not cancelling big events like England Rugby, Cheltenham and footie matches (Liverpool vs AC Madrid would you believe) epitomises the delay in making the right decisions early.
Get ready for lots of excuses. A little honesty, humility even, really would go a long way.
Centralisation
Central diktats applied in blanket form to the whole country are sometimes necessary but local and regional voices have been marginalised by Chinese-style levels of over-centralisation. The situation in Devon and elsewhere is very different from London, decisions here would have been different too.
In a way all outbreaks are local and the marginalisation of local authorities and their capability to test and trace has made action on the ground difficult.
There will be reasonable calls for devolved power to the regions in the same way as in Scotland Wales and Northern Ireland. COVID19 gives this argument lots of ammunition.
Decision making It sometimes seems that decision making has made on the hoof and entirely within Number 10. Delay, uncertainly and perhaps lack of urgency meant windows of opportunity were closed before the political curtains were even pulled back.
It sometimes seems that decision making has made on the hoof and entirely within Number 10. Delay, uncertainly and perhaps lack of urgency meant windows of opportunity were closed before the political curtains were even pulled back.
We have to admit that “closing Heathrow” wont have been an easy call, but the needs were clear long before the decisions were made.
Flattening the curve is the least ambitious aspiration as compared to reducing the total numbers affected.
Messages on reducing individual risk have been absent.
Press briefings For many of us, the daily press briefings have been a crafted balancing act between self congratulation and dutiful expression of grief. However, over-emphasis on back slapping and gratitude has detracted from objectivity.
For many of us, the daily press briefings have been a crafted balancing act between self congratulation and dutiful expression of grief. However, over-emphasis on back slapping and gratitude has detracted from objectivity.
They might had had the function of lifting the nations morale but have veered too far towards becoming party political broadcasts with legal teams in the background yelling “Don’t admit to anything!”
I have lost count of the times I have heard the lines:
- “Thank you everybody for doing everything”
- “At all times we are following the science”
- “We are going to flatten the curve”
- “We have made the right decisions at the right time”
Most days I tuned in from the relaxed ambience of my greenhouse at 5pm. Yet even there my heart rate increased in frustration as I listened. Our high mortality, fat curves and slow decision making make confident assertions of success irritating. I have more than a niggling worry that our response to future challenges will be compromised by inability to admit to recent mistakes.
The briefings had not even hinted that COVID19 risk factors can be reduced. Stopping smoking, reducing weight, eating well, exercising and getting enough Vitamin D would not only flatten the curve, but also reduce its height and thus overall deaths.
The dramatic effect of poverty, social inequality and the impact on the BAME community are cans which have been kicked down the road.
This was a glorious opportunity, with the nation attentive, to motivate improvements in health enhancing action and has been sadly missed.
The reality is more stark and with COVID19 as unforgiving as nature itself, these lessons need to be learned.
Late lockdown. 
Early lockdowns suppress the pandemic to low levels with manageable subsequent outbreaks. Late lockdowns work less well. There are questions being asked about whether our lockdown had any effect at all on disease trajectory at all.
This all highly theoretical yet will be a feature of calls suggesting that lockdowns are ineffective and wrong, even if it could not be more clear they work well if done well.
Even late lockdowns might be better than nothing, as can be seen by the low rates in regions like the South-West, even if the overall aim is to flatten the curve rather than making it smaller.
Testing and tracing in the UK
This was abandoned at the worst time possible – Mid March.
Perhaps they realised the genie was out of the bottle, but you might be forgiven to thinking that this was the herd-immunity dogma in action: “Don’t put out the little fires, let it go big and burn itself out”
Such nonsensical decision making is more likely with the pathological over-centralisation of power in the UK. Ongoing testing and tracing would have continued to work well in areas less overwhelmed than London and even in the metropolis public sector services could have been rapidly developed if this was the decision at the time.
Now we risk repeating the same mistakes with over-reliance on unproven technology from our gadget-friendly health secretary, who seems too keen on risky novelty rather than building on current resources in the NHS and Public Health.
Contracts are flowing to the usual private sector chums and donors who will take up the task of testing and tracing using low paid staff and off shore finance. Literally no change there.
The other practical concern is that once this pandemic is over, the testers will be dispatched and teams dismantled, losing the opportunity to develop built in public sector systems ready to go next time.
Procurement
Buying stuff we need has been at best chaotic and beset with cock-up’s.
The global scramble for kit might have made this problematical, but our stores of PPE were at inadequate levels, and some out of date due to cost and corner cutting. Again, over centralised decision making has shown its weaknesses, as has global supply lines and our own manufacturing short-fall.
One of the worst moments of the press briefings was the Home Secretary’s pseudo-apology to PPE-light health care workers, the most basic mistake for anyone familiar with conflict resolution. “I’m sorry if you think you haven’t had enough PPE”.
The various cock ups amid the chaos are well described in the media, but at their heart lay poor preparation.
Care homes and carers.
In our understandable haste to beef up the hospitals for the presumed onslaught, we missed out on looking after the most vulnerable in our institutions and those who care for them.
It might seem insane in looking back, but systems as they stood meant patients recovering from infections were sent into care homes while infectious. Infection was also spread by agency staff moving from home to home to fill in the many gaps opened up by self isolation of regular staff as well as usual recruiting problems.
The isolated nature of Care Homes is also highlighted by COVID19 as a big problem. Lack of a co-ordinated approach to or by them seems almost inevitable when you consider there are 5,500 different providers operating 11,300 homes in the UK.
Along with lack of PPE and testing this led to excess and avoidable mortality.
In Plymouth many care homes have maintained a COVID free environment by planning way ahead of ponderous central diktat. It would be wise to ensure that all admissions to nursing homes are COVID free and discharges from hospital to sites offering intermediate levels of care to look after recovering COVID patients to ensure this.
The Big Questions…
Did our lockdown make any difference?
The lockdown achieved its aim of preventing the overwhelming of health services, and it seems to have spared areas far from international transport hubs. But done late, it has not controlled the problem in the way we would have liked.
It might also have allowed many vulnerable people to shield from risk and perhaps this is the main reason the health services have been able to cope.
While denying that herd immunity was the aim, that is now in effect what we seem to be heading very slowly towards.
Given to that the health services have learned fast how to manage cases and their own systems, we need to ask if an another national summer lockdown would be of any benefit.
The long game is getting levels low enough to be able to extinguish local outbreaks. As we head for June, we are still not there as a nation, and certainly not globally, but lockdowns need to be done well to work. That means early and local.
Is next winter is the big issue?
Coronaviruses are generally highly seasonal, so the falls in infection rates we are now seeing might well be, in part at least, a feature of their biology as well as our response.
Putting that aside, even if we continue with the current rate of 2-3000 new cases a day will mean that by the start of the flu season (October to May) we will have another 450,000 infected people in the UK which leaves us a long way from herd immunity and thus leaving most of the population vulnerable.
If we continue or repeat the lockdown into the summer, then we might reduce the number of summer cases, but also increase the number of people still to be infected when winter (and flu season) comes along. What then? Another rapid and more total lockdown? That will be difficult economically, politically and for the vast majority of the population.
What do we do now?
The excellent independent “iSAGE” group set up to give advice truly uninfluenced by political pressure, have published recommendations on how to proceed from here. It’s a long read and so a summary might be of use. Clarity will be wonderful in these times of uncertainty.
Ease the lockdown as soon as our capacity to deal with subsequent outbreaks is in place.
Restrict high risk activities like needless travel and control potential cases coming into the country.
Reduce outbreaks by restricting large gatherings and maintaining physical distancing.
Protect at risk groups and keep them COVID free with the hope that a vaccine will come along, that treatment will be developed or that herd immunity will be achieved.
Protect care homes and crowded institutions They are a national priority and new isolation hospitals should be developed over the summer to ensure that our care homes, are kept COVID- free during the winter.
Beef up public health. I’m worried that we continue to be dominated by our tech-heavy human-light over-centralised and heavily privatised approach. The list of cock-ups is increasing, driven in part by vain innovation alone instead of making the best of our present under-used and uncoupled public and primary care teams and networks.
Get ready for the winter wave and assume we will have a nasty flu outbreak in tandem with resurgence of COVD19 from October through the winter. That means individually as well the health service and society at large. Planning needs to consider the worst case scenario
Develop better treatments and vaccines – hope for a vaccine is steadily increasing, but remains fraught with difficulty, there is a possibility it may never arrive. Treatments that make a real difference might be in the pipeline, but none have emerged as yet. (More on this soon)
Globalise our response to future pandemics, that means a better EU and WHO as well as the many other networks developing out of the COVID experience. Much of this is happening in the science sector.
Well done…….
For anyone who has read till this point, well done! It is rather hard to keep this brief, but that has been my little overview of COVID till now.
Hope for the best. This is a useful strategy to help us all keep sane in this ever more challenging world. It has been described by therapists as a good fall back position for anyone who is struggling with the many problems the pandemic has brought.
Who knows, the best case scenario might happen, it might just die out in the summer.
Worth hoping for, but not planning for.


Thanks for the kind words Tricia, I shall keep writing and develop the links with agribusiness, climate change, transport and all our previous worries. Hope you're well.
Thanks Ian. Hope all is well. I'm looking up some rain dances!
Great reporting Colin, thank you. You are becoming my 'go to' blog for honest, well researched information. Stay well and I hope we may meet again soon.
Excellent analysis, Dr Bannon.